What is Osteoarthritis?
Osteoarthritis (OA) is a degenerative joint disease and is one of the most common types of arthritis. Often people think of this disease as a ‘wear and tear’ arthritis. In OA, the smooth cartilage between the joints starts to break down and is no longer able to regenerate. This can lead to a decrease in space between joints. OA affects the entire joint, involving the bones, the muscles, ligaments, and capsule that surround the area. It can cause joint pain, stiffness, decrease in function, and can greatly affect a person’s quality of life.
OA can affect anyone; however, it is more common in females and becomes more common as you age. The exact cause of OA is unknown, but multiple factors can contribute to the cause of OA. The risk of developing OA increases with age, with people being over the age of 50 at an increased risk. Other factors such as a previous injury to a joint, weak musculature, obesity, overuse of joints, and genetics, can all play a role in being at risk for OA. The most common areas that are affected are the joints of the knees, hips, hands, and back.
Now you might be wondering, how can a chiropractor help me with my OA? Chiropractors are excellent at diagnosing, treating, and managing conditions involving your bones, muscles, joints, and nervous system. Making chiropractors a great option to help manage your condition. There are many different signs and symptoms a chiropractor will look for on your first visit that can indicate OA. Signs and symptoms that could indicate OA include persistent pain, limited morning stiffness, reduced function, crepitus (abnormal crackling of a joint), restricted movement, and bony enlargements. Contrary to many beliefs, an X-ray is not needed to diagnose OA, however, it can be helpful to confirm a diagnosis in moderate and advanced cases. X-rays may also be useful to rule out other conditions. OA is primarily a clinical diagnosis that your chiropractor can help treat and manage.
Tips for Living with Osteoarthritis:
Unfortunately, there is no cure for OA. The condition progresses as you age and can become worse. However, there are many treatment options that you can do to help prevent or minimize pain and maintain your function. The first line of treatment is education, exercise, and weight control. The second line of treatment in combination with the first is using passive treatment from a therapist and/or pharmacological pain relief. The final line of treatment after trying other treatments is surgery. 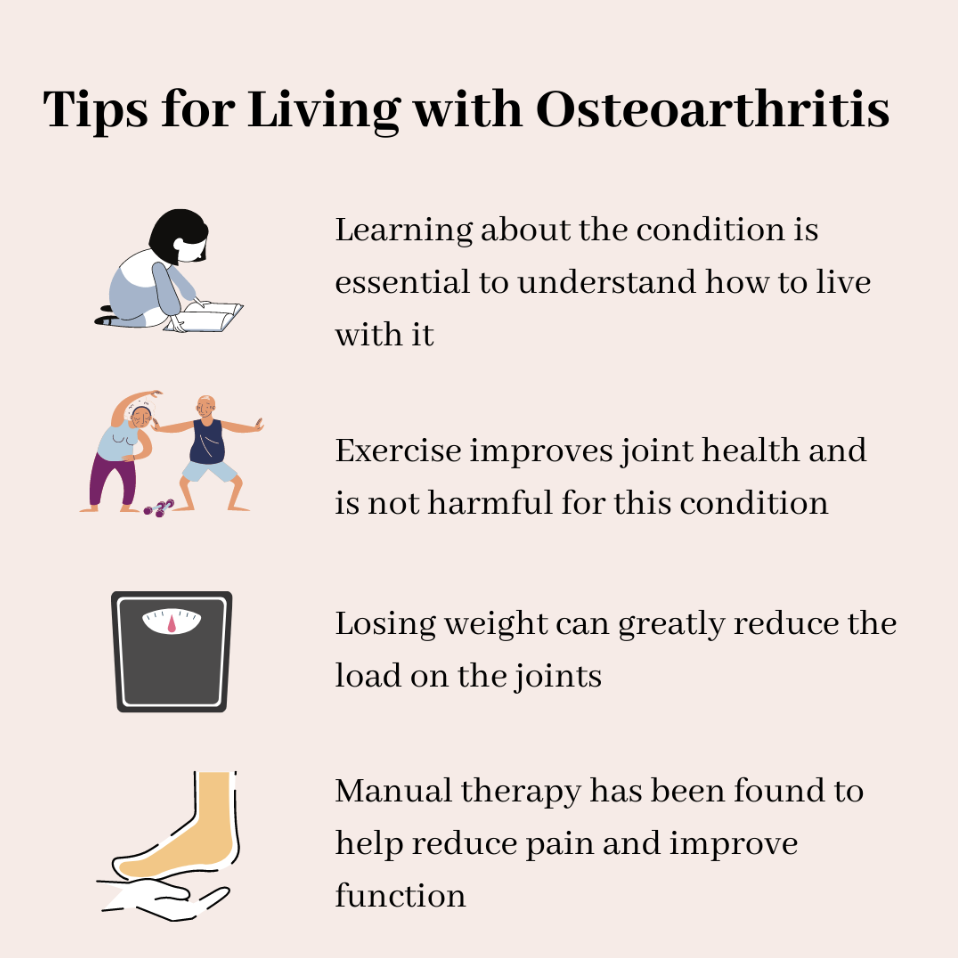
Education. The more you know about OA, the better you will be able to live with it and care for yourself. Seeking out help from a health professional is an important step when managing this condition. A health professional can give you guidance and information that you need to live a better quality of life.
Exercise. Clinical guidelines recommend exercise as one of the primary treatments for OA. It may seem counterintuitive that loading your joints and exercise can be beneficial. However, research has shown that exercise is not harmful in people with or at risk of OA and is very good for joint health. Exercise for the management of OA includes strength training, sensorimotor control training, and functional stability training.
Weight loss. Obesity is one of the most important modifiable risk factors for OA. An increase in body weight increases the load and stress being put on your joints. The knee supports 3-5 times your body weight, therefore, losing 1 kg of body weight would lead to a 10% decrease in your risk of knee OA! Weight loss plays a huge role in decreasing joint loads. This can help decrease your pain and increase your function when you are living with OA.
Manual therapy. Clinical guidelines recommend manual therapy in conjunction with other therapies (such as exercise) to treat OA. Manual therapy can include joint mobilizations and stretches to help increase range of motion and increase function.
Pharmacological treatment. Anti-inflammatory and pain medications, as well as injections, can be an option for pain relief and decreasing stiffness. These types of medications should only be considered if other non-pharmacological approaches did not control symptoms, and individuals should speak to their primary care physician or pharmacist about this.
Surgery. Patients who have severe disability, persistent pain despite multiple types of treatment, or require regular pain medication, should be referred to a surgeon. This is the last line of treatment for OA and all other types of treatment should be tried before this option.
References:
1. BMJ Best Practice. Osteoarthritis – Symptoms, diagnosis and treatment | BMJ Best Practice [Internet]. 2020 [cited 2020 Aug 17]. Available from: https://bestpractice.bmj.com/topics/en-gb/192?q=Osteoarthritis&c=suggested





